Mastitis is inflammation of the breast that can occur during lactation.
There are different hypotheses as to why this inflammation occurs. One, is a narrowing of the milk ducts due to congestion and inflammation. Specifically, hyperlactation or a disruption of the breast microbiome [1].
Alternatively, mastitis may be due to pressure inside the alveoli and milk ducts. This pressure may break the connections between the milk-producing cells and the ductal cells, causing inflammation and swelling. The immune system responds by increasing white blood cells, which changes the milk’s composition and increases inflammation [2].
Mastitis is part of a spectrum of conditions that range from mild inflammation to bacterial infection [1].
Spectrum Conditions
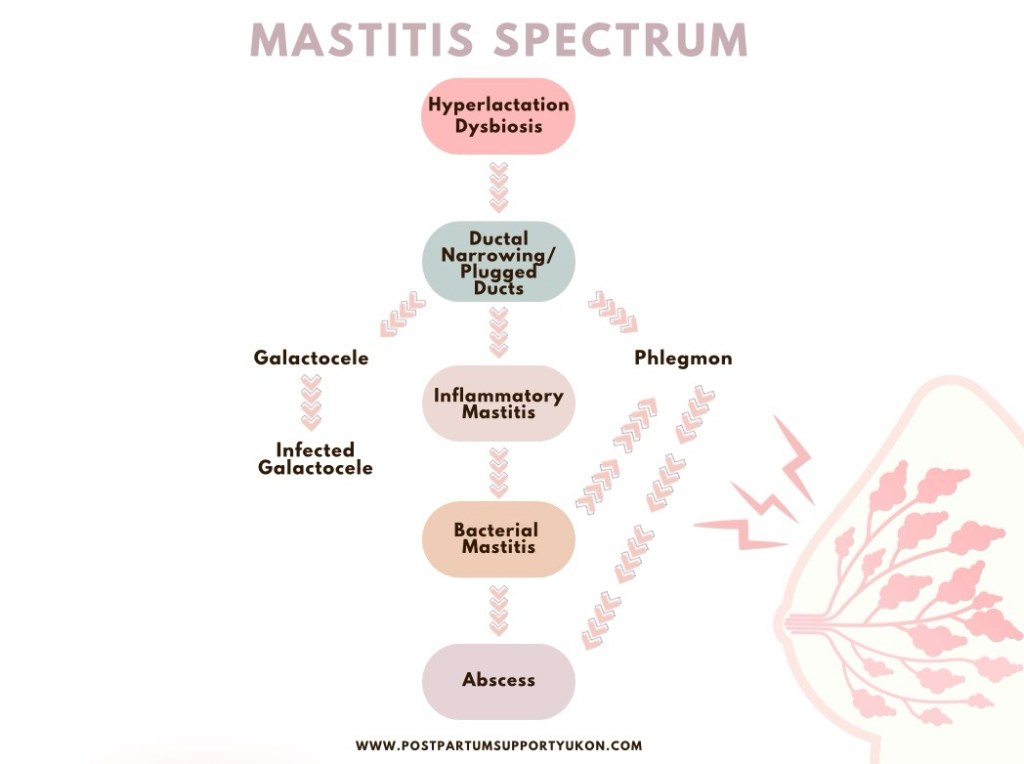
Plugged Duct or Ductal Narrowing
- Inflammation and narrowing of the milk ducts resulting in pain/tenderness. It’s important to note that there is no “plug” that you have to squeeze out.
Inflammatory Mastitis
- More significant breast inflammation with pain, redness, and swelling. There is often no infection, but it can progress into one. No antibiotics are needed, but ibuprofen or acetaminophen may help pain and swelling. In addition to rest and cold packs.
Bacterial Mastitis
- A progression from ductal narrowing and inflammatory mastitis to bacterial mastitis, which requires antibiotics. Bacterial mastitis is not contagious and does not pose a risk to your baby. You can continue to nurse as normal.
Phlegmon
- A firm, mass without clear, discrete fluid collection, often due to untreated or worsened mastitis. However, it can also result from excessive deep tissue massage.
Abscess
- An abscess is a progression from bacterial mastitis or phlegmon to an area of infected fluid collection that requires drainage. Approximately 3–11% of women with acute mastitis will develop an abscess.
Galactocele
- A galactocele develops when ductal narrowing obstructs the flow of milk. As a result, the milk collects and forms a cyst, which presents as a lump. The lump may fluctuate in size throughout the day and it may be smaller after a feed. A galactocele may be uncomfortable, but it is not usually painful. It can become infected.
Subacute Mastitis
- Chronic inflammation due to an imbalance in the breast microbiome (mammary dysbiosis), often with burning pain or recurrent symptoms.
Recurrent Mastitis
- Multiple episodes of mastitis, often due to unresolved underlying causes such as oversupply, dysbiosis, or ineffective milk removal.
Causes
- Hyperlactation or oversupply
- e.g., excessively emptying the breast, missed feeds, scheduled or timed feeds, oral function issues, poor latch and positioning, ineffective pump, poor flange fit, abrupt weaning, genetics…
- Dysbiosis (i.e., disrupted breast microbiome)
- e.g., genetics, use of antibiotics and probiotics, regular breast pump usage, and c-section births…
- Pressure inside milk-producing structures (alveoli and ducts)
- e.g., external pressure (tight bra, sleeping positions), engorgement, hyperlactation or oversupply, excessively emptying the breast, missed feeds, scheduled or timed feeds, oral function issues, poor latch and positioning, ineffective pump, poor flange fit, abrupt weaning, previous breast surgery…
Multiple factors contribute to the development of mastitis and its potential progression.
Symptoms
- Pain, heat, and swelling in the affected area
- A sore lump or tender spot
- Color changes to the skin (e.g., redness, red streaks, brown or purple). Color changes can be harder to detect in dark skin tones.
- Flu-like symptoms (i.e., achy, tired, chills, fever, feeling run down).
Treatment
- Continue nursing on demand or about 8-12 feeds in 24 hours.
- Ice or cold packs to the affected area.
- Take ibuprofen or acetaminophen to reduce pain and swelling (as directed by your health care provider or pharmacist).
- Rest.
- Lymphatic drainage or “breast gymnastics.”
- If you are experiencing engorgement, pump or hand express (preferred) until you feel comfortable.
- Wear a comfortable and supportive bra. Nothing too tight that places excessive pressure on the breast tissue.
If you have concerns around your supply, weaning, pump usage, flange fitting, oral function, positioning, latch, or any other concerns, please consider reaching out to a lactation specialist.
Avoid:
- Antibiotics unless you have bacterial mastitis. Home care, as noted above, is usually all that’s needed.
- Trying to “empty” the breast. This includes overexpressing such as, over pumping, pumping after feeds, and additional feeds. Feeding on demand or following your normal pumping schedule is sufficient. Placing more demand on the breast could increase inflammation.
- Deep tissue massage and massagers, which may increase inflammation. There is no “plug” that you have to squeeze out.
- Heat or use heat sparingly. Heat may increase inflammation.
- Sleeping on your chest or situations where there is added pressure on your chest.
- Tight bras or clothing that may put pressure on your chest.
- Timed or scheduled feeds. If you are looking to wean, please do so slowly. It may be helpful to speak with your health care provider or lactation specialist to support you in establishing a plan for weaning.
When To Seek Medical Help
- Symptoms persist for more than 24-48 hours despite home treatment.
- Symptoms worsen or you feel extremely unwell.
- You develop a high fever (over 100°F).
Need More Help?
Consult a lactation consultant or healthcare provider for personalized support. Mastitis can be managed effectively with early intervention and proper care.
References
[1] Mitchell, K. B., Johnson, H. M., Rodríguez, J. M., Eglash, A., Scherzinger, C., Zakarija-Grkovic, I., Cash, K. W., Berens, P., Miller, B., & the Academy of Breastfeeding Medicine. (2022). Academy of Breastfeeding Medicine clinical protocol #36: The mastitis spectrum, revised 2022. Breastfeeding Medicine, 17(5). https://doi.org/10.1089/bfm.2022.29207.kbm
[2] Douglas, P. (2022). Re-thinking benign inflammation of the lactating breast: Classification, prevention, and management. Women’s Health, 18, 17455057221091349. https://doi.org/10.1177/17455057221091349
DISCLAIMER: The content of Postpartum Support Yukon‘s website does not constitute medical advice. This page is an overview and does not contain all possible information about mastitis. If you have concerns about any health or medical condition, medications, diagnosis, or treatment, please consult with a licensed healthcare provider or other relevant professional. If you are experiencing a medical emergency, please contact your health care provider, local emergency department, 911 or your local emergency number immediately. Postpartum Support Yukon is intended for informational purposes only.
